Fighting Antimicrobial Resistance Takes All of Us
Today we kick off U.S. Antibiotic Awareness Week, held nationwide every year from November 18–24. Even though the week is titled "Antibiotic" Awareness Week, the CDC emphasizes responsible use of both antibiotics and antifungals, because antimicrobial resistance (AMR) affects bacteria and fungi alike.
AMR remains one of the most serious global health threats. The CDC estimates that in the U.S. alone, antimicrobial-resistant infections cause more than 2.8 million illnesses and over 35,000 deaths each year.
Why Appropriate Use Matters
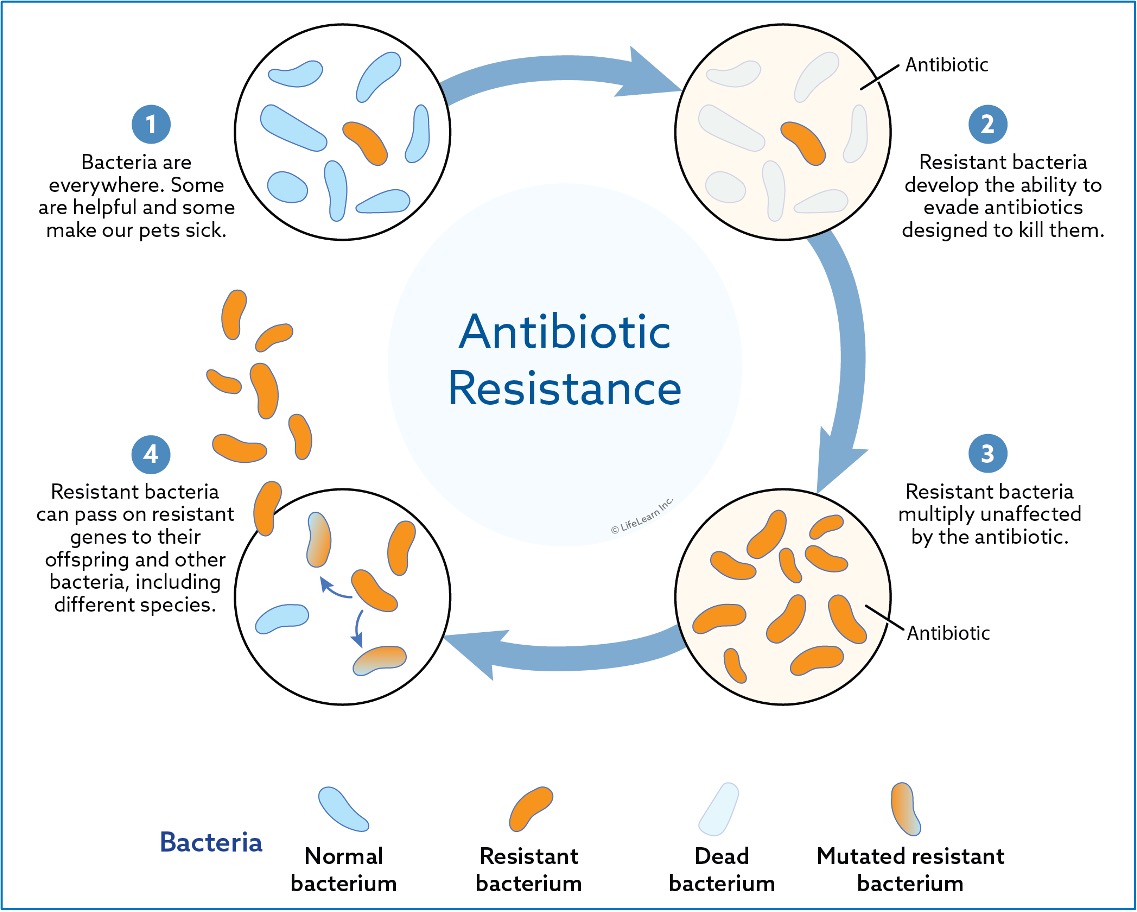
One of the most important things to remember is that antibiotics treat bacterial infections-not viral infections. They are effective for illnesses such as strep throat or urinary tract infections, but not for colds, flu, RSV, or most sore throats.
If you're feeling unwell, resist the urge to ask your doctor for antibiotics. Instead, let your doctor evaluate what's actually making you sick and whether an antibiotic is needed. Taking antibiotics when they aren't necessary, or taking them longer than prescribed, teaches bacteria how to survive-driving the development of resistance.
Vaccination is also a powerful tool. By preventing infections in the first place, vaccines reduce the need for both antibiotics and antifungals.
Antifungal Resistance is Also Rising
Antimicrobial resistance includes more than bacteria. Fungi can also develop resistance to antifungal medications. Emerging pathogens like Candida auris are becoming more difficult to treat and illustrate why appropriate antifungal use is equally important.
A One Health Perspective
AMR is a One Health issue because resistant microbes move across people, pets, livestock, wildlife, food systems, and the environment.
In U.S. food-animal production, a substantial share of antibiotic sales are for livestock, including many that the FDA classifies as medically important antibiotics-drug classes that are essential for treating bacterial infections in humans (such as penicillins, cephalosporins, fluoroquinolones, macrolides, tetracyclines, and aminoglycosides).
Regulatory changes have greatly reduced the use of antibiotics for growth promotion, but concerns remain about non-therapeutic use contributing to resistance. Resistant bacteria from food-animal environments can potentially move through the food chain or through environmental pathways.
What about our pets?
The risk of pets transmitting antimicrobial-resistant bacteria to people appears to be low based on current evidence. Still, thoughtful antibiotic use in veterinary medicine, good hygiene, and routine preventive care help safeguard everyone in the household.
What We Can All Do
- Only use antibiotics or antifungals when genuinely needed.
- Take them exactly as prescribed-no skipping doses, no sharing, no saving for later.
- Keep vaccinations up to date for yourself, your family, and your pets.
- Practice good hygiene, including safe food handling and regular handwashing.
- Talk with your doctor or your veterinarian about when antimicrobial treatment is appropriate.
Fighting antimicrobial resistance truly takes all of us.
Thank you for being part of this community and for the work you do to support families and their pets.
https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
https://www.cdc.gov/antimicrobial-resistance/about/index.html
https://www.cdc.gov/antimicrobial-resistance/communication-resources/usaaw.htmlwareness Week (USAAW) Toolkit | Antimicrobial Resistance | CDC
https://pmc.ncbi.nlm.nih.gov/articles/PMC4520913/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4638249/
https://pmc.ncbi.nlm.nih.gov/articles/PMC10336692/
------------------------------
Michael J Blackwell, DVM, MPH, FNAP
Assistant Surgeon General, USPHS (Ret.)
Director, Program for Pet Health Equity
University of Tennessee
https://pphe.utk.edu
------------------------------